

|
Dr. Fessy Louis T |
Dept. of Reproductive Medicine & Surgery, |

Prof. Alka Kriplani
M.D., FRCOG, FAMS, FICOG,
FIMSA, FICMCH, FCLS
Dept. of Reproductive Medicine & Surgery,
AIMS – AMRITA Institute of Medical Sciences, Kochi
FOGSI All India Vice President 2021-22
ICOG- Governing Council Member
ISAR- National Executive Member
Obstetrician: The First Doctor of Life
As mentioned by Prof. CN Purandare, the past president of FIGO and a respected gynaecologist and obstetrician with more than 45 years of experience, “A Doctor’s life is a fascinating journey of several ups and downs, of feelings, making a difference in the lives of those who have placed their precious lives in their hands.”1 In context, this becomes more stimulating for an obstetrician as he or she have to deal with the two lives i.e., of the baby and mother. Regardless of the child’s gender, it is the first encounter for her/him with a doctor who facilitates its journey and transition from the womb to the external world.
Nevertheless, the practice of an obstetrician is extremely demanding in a country like India where about 37,000 obstetricians need each single one to deliver or supervise average 800 deliveries; while it is well-known that anything > 200–300 per year deliveries can be a physical, mental and emotional nightmare for any for an obstetrician.1
This pressure often gets further compounded by the expectations of the would be parents. Yet, in the end it is extremely satisfying for most obstetricians caring for two lives at once; especially considering the fact that obstetric care offers a critical window of opportunity to facilitate and ensure happy outcomes for both the mother and the child in both
short- and long-term. In this short review, we discuss about the need and importance of apposite nutrition during the “First 1000 days of life”.
Obstetrician: The First Doctor of Life
As mentioned by Prof. CN Purandare, the past president of FIGO and a respected gynaecologist and obstetrician with more than 45 years of experience, “A Doctor’s life is a fascinating journey of several ups and downs, of feelings, making a difference in the lives of those who have placed their precious lives in their hands.”1 In context, this becomes more stimulating for an obstetrician as he or she have to deal with the two lives i.e., of the baby and mother. Regardless of the child’s gender, it is the first encounter for her/him with a doctor who facilitates its journey and transition from the womb to the external world.
Nevertheless, the practice of an obstetrician is extremely demanding in a country like India where about 37,000 obstetricians need each single one to deliver or supervise average 800 deliveries; while it is well-known that anything > 200–300 per year deliveries can be a physical, mental and emotional nightmare for any for an obstetrician.1
This pressure often gets further compounded by the expectations of the would be parents. Yet, in the end it is extremely satisfying for most obstetricians caring for two lives at once; especially considering the fact that obstetric care offers a critical window of opportunity to facilitate and ensure happy outcomes for both the mother and the child in both
short- and long-term. In this short review, we discuss about the need and importance of apposite nutrition during the “First 1000 days of life”.
Relationship between your prenatal and adult life: “Barker hypothesis”
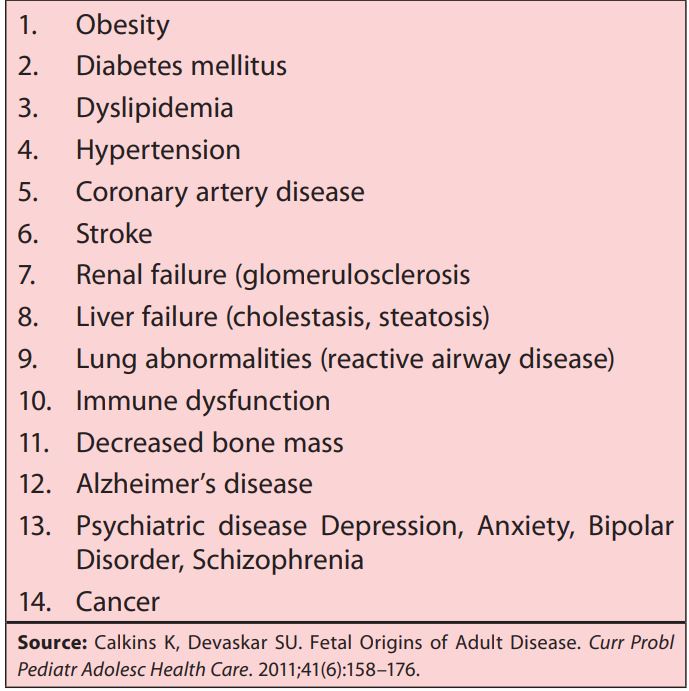
The “Barker hypothesis” is a near exact impression that provides a glimpse of the importance of early life care and well-being. Dr. David Barker first popularized the concept of “Fetal origins of adult disease (FOAD)”, also popularly known as the “Barker hypothesis”.2 Since its inception, the FOAD hypothesis has received considerable attention. It basically holds that events during early development of a child have a profound impact on his/her risk for development of future adult disease. Low birth weight, a surrogate marker of poor fetal growth and nutrition, and a proxy for intrauterine growth retardation (IUGR), is linked to various chronic diseases like coronary artery disease (CAD), hypertension, obesity, insulin resistance, and type 2 diabetes (Table 1).2,3 These relationships are further modified by patterns of postnatal growth; with “fetal developmental programming by nutritional stimuli” being one of the most widely accepted mechanisms thought to underlie these relationships.4,5
Day 25100140280Birth3103706401000
Table 1: Chronic diseases associated with the “Barker hypothesis” (Chronic diseases attributed to “Developmental Origins”)2

Common nutritional deficiencies in pregnancy:
The menace of hidden hunger
Hidden hunger is referred to as the presence of nutritional deficiencies, which can occur without a deficit in energy intake as a result of consuming an energy-dense, but nutrient-poor diet.6,7 The nutritional deficiency manifests in the form of micronutrient deficiencies, or the lack of essential vitamins and minerals that the body needs to sustain life.6 The burden of hidden hunger during pregnancy remains an important concern since pregnancy is associated with physiologic changes that result in decreased concentrations of circulating nutrient-binding proteins and micronutrients.8,9
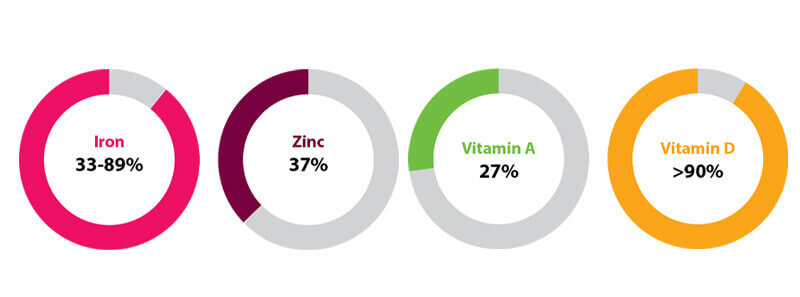
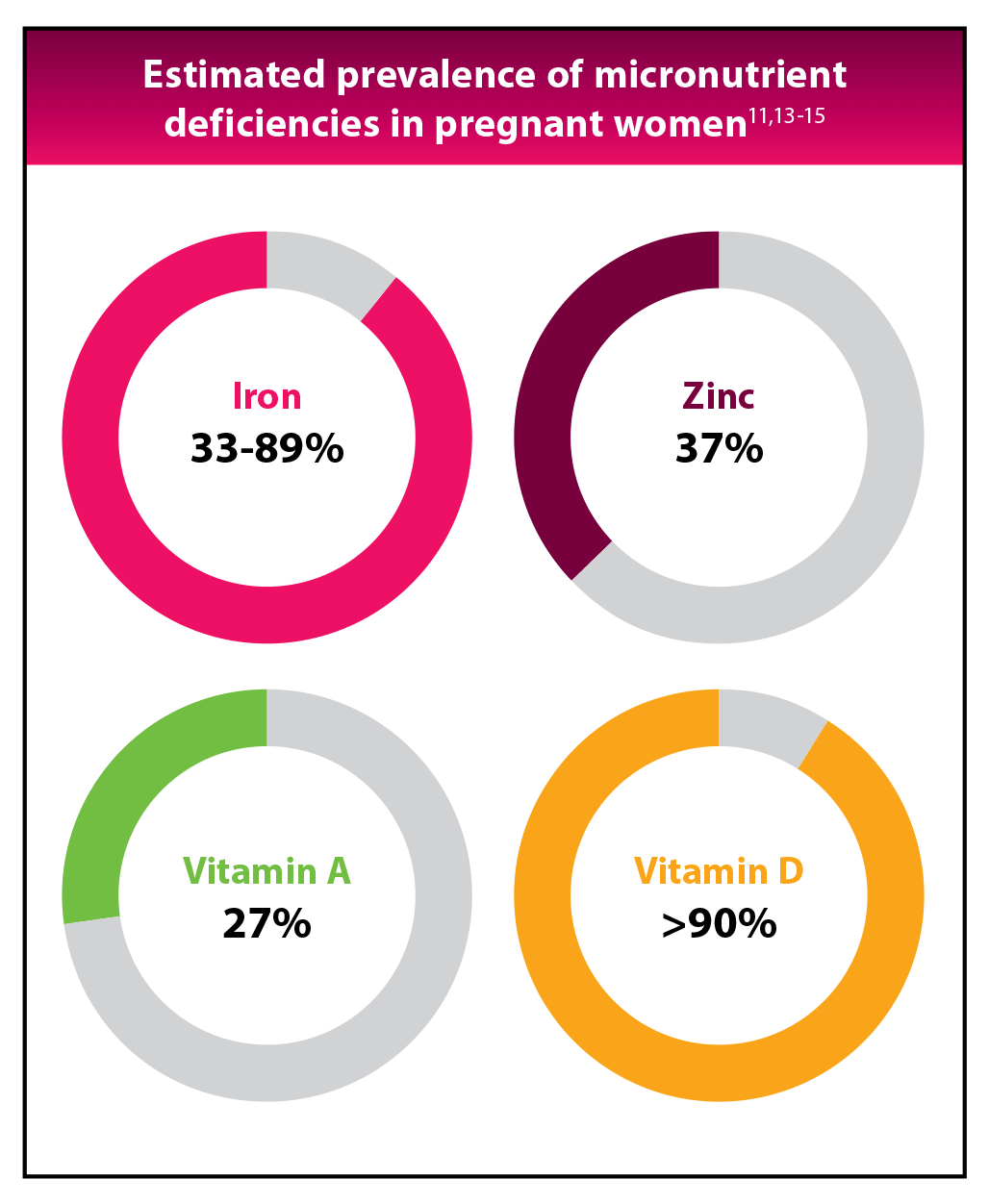
Several reports have confirmed increase in the requirement of many micronutrients and vitamins in pregnancy.1Anemia due to iron deficiency is one of the most prevalent micronutrient deficiencies globally.10 In the Indian population, the prevalence of anemia has been estimated to range from 33% to 89% among pregnant women.11 Anemia during pregnancy has been found to be associated with increased risk of maternal mortality, perinatal mortality, and infants with low birthweight (LBW).10
Multiple micronutrient deficiencies:
A growing concern for perinatal health
Besides the high prevalence of iron deficiency, data from developing nations have shown that multiple micronutrient (MMN) deficiencies including those of, but not limited to, vitamin A, zinc, vitamin B12, iodine and folate often coexist among women of reproductive age. They are exacerbated in pregnancy due to the increased demands of the developing fetus, leading to potentially adverse effects on the mother and baby.10,12 Data accrued from studies conducted among pregnant women in India suggest the prevalence of zinc deficiency to be 37%, vitamin A deficiency to be 27%, and vitamin D deficiency to be more than 90%.13-15
Estimated prevalence of micronutrient deficiencies in pregnant women11,13-15
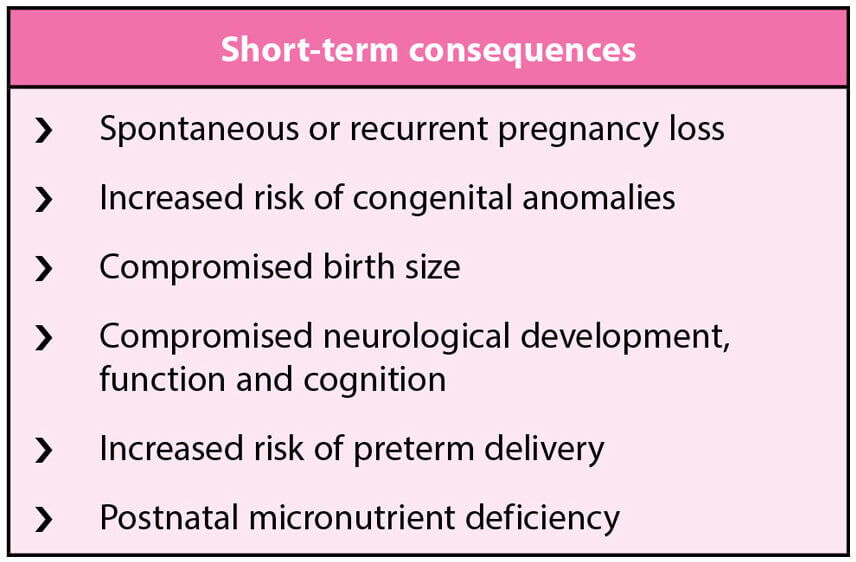
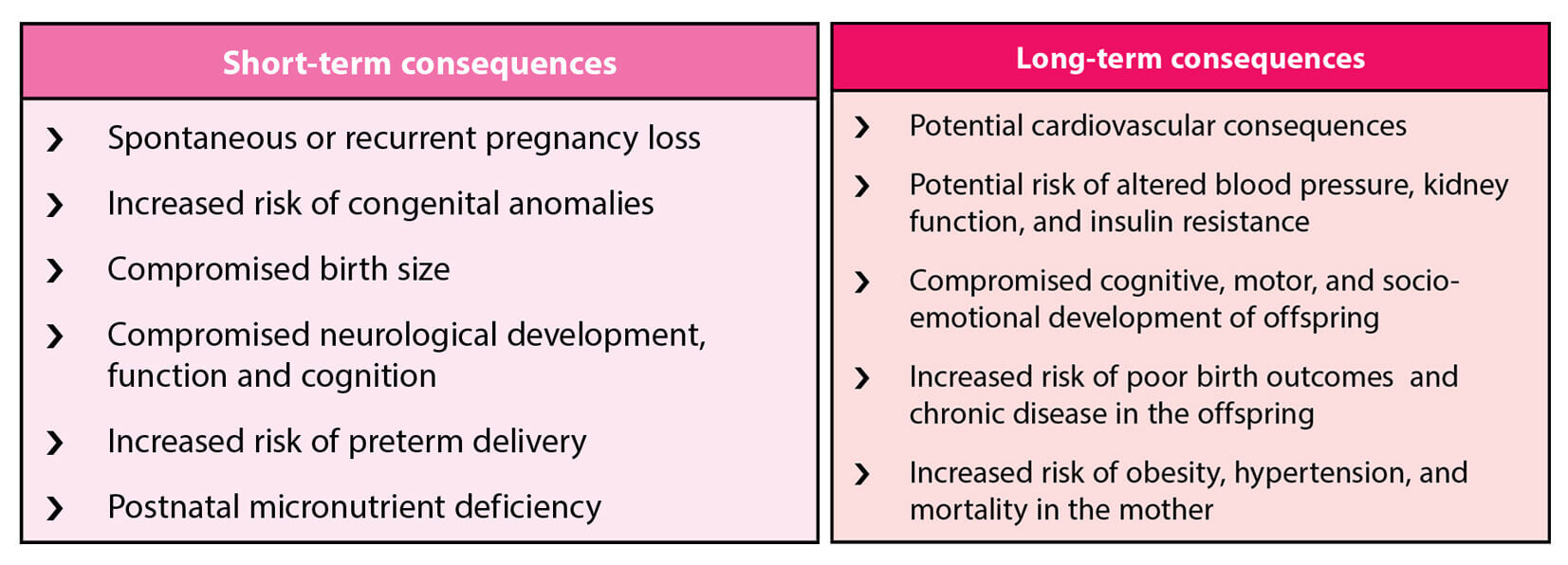
Short- and long-term consequences
of maternal MMN deficiency
Inadequate maternal micronutrient status during the second and third trimesters of pregnancy might compromise birth size. Nutritional inadequacies of the developing fetal brain and central nervous system might compromise neurological development, function and cognition. Inadequate maternal nutritional status, including micronutrients, increases the risk of poor birth outcomes, and chronic disease in the offspring; and obesity, hypertension, and mortality in the mother (Table 1).2,9
Table 1: Short- and long-term consequences of maternal MMN deficiency
Short-term consequences
- Spontaneous or recurrent pregnancy loss
- Increased risk of congenital anomalies
- Compromised birth size
- Compromised neurological development,
function and cognition - Increased risk of preterm delivery
- Postnatal micronutrient deficiency
Long-term consequences
- Potential cardiovascular consequences
- Potential risk of altered blood pressure, kidney
function, and insulin resistance - Compromised cognitive, motor, and socio-
emotional development of offspring - Increased risk of poor birth outcomes and
chronic disease in the offspring - Increased risk of obesity, hypertension, and
mortality in the mother
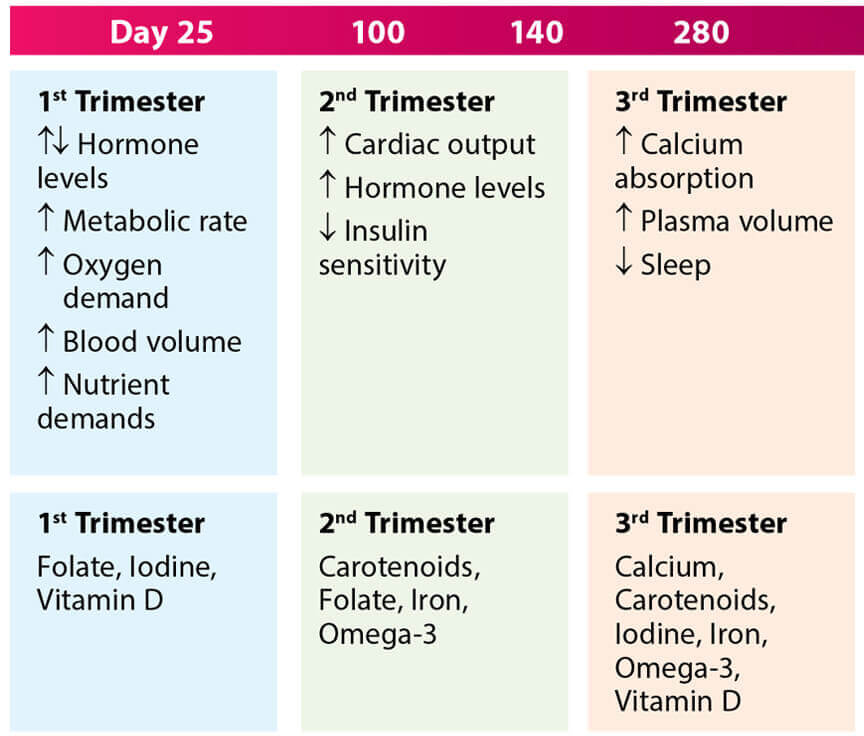
First 1,000 days of nutrition: Critical window for child’s optimum health and development
The first 1000 days of life refers to the period from conception through the child’s second birthday.4 This period is very crucial for the growth and development of the fetus and child and its long-term health outcomes.5 Adequate nutrition and care during this time is vital for supporting critical periods of fetal growth and development, maternal health, and for promoting infant and toddler growth. Failure to provide key nutrients during the first 1000 days of life can result in developmental shortfalls such as a lifelong deficit in brain function and chances of developing nutrition-related non communicable diseases.4,5
Maternal changes and key nutrients required during first 1000 days of life4

Common nutritional deficiencies in pregnancy: The menace of hidden hunger
Hidden hunger is referred to as the presence of nutritional deficiencies, which can occur without a deficit in energy intake as a result of consuming an energy-dense, but nutrient-poor diet.6,7 The nutritional deficiency manifests in the form of micronutrient deficiencies, or the lack of essential vitamins and minerals that the body needs to sustain life.6 The burden of hidden hunger during pregnancy remains an important concern since pregnancy is associated with physiologic changes that result in decreased concentrations of circulating nutrient-binding proteins and micronutrients.8,9
Several reports have confirmed increase in the requirement of many micronutrients and vitamins in pregnancy.1Anemia due to iron deficiency is one of the most prevalent micronutrient deficiencies globally.10 In the Indian population, the prevalence of anemia has been estimated to range from 33% to 89% among pregnant women.11 Anemia during pregnancy has been found to be associated with increased risk of maternal mortality, perinatal mortality, and infants with low birthweight (LBW).10
Multiple micronutrient deficiencies: A growing concern for perinatal health
Besides the high prevalence of iron deficiency, data from developing nations have shown that multiple micronutrient (MMN) deficiencies including those of, but not limited to, vitamin A, zinc, vitamin B12, iodine and folate often coexist among women of reproductive age. They are exacerbated in pregnancy due to the increased demands of the developing fetus, leading to potentially adverse effects on the mother and baby.10,12 Data accrued from studies conducted among pregnant women in India suggest the prevalence of zinc deficiency to be 37%, vitamin A deficiency to be 27%, and vitamin D deficiency to be more than 90%.13-15
Estimated prevalence of micronutrient deficiencies in pregnant women11,13-15
Short- and long-term consequences of maternal MMN deficiency
Inadequate maternal micronutrient status during the second and third trimesters of pregnancy might compromise birth size. Nutritional inadequacies of the developing fetal brain and central nervous system might compromise neurological development, function and cognition. Inadequate maternal nutritional status, including micronutrients, increases the risk of poor birth outcomes, and chronic disease in the offspring; and obesity, hypertension, and mortality in the mother (Table 1).2,9
Table 1: Short- and long-term consequences of maternal MMN deficiency
Table 2: The United Nations International Multiple Micronutrient Antenatal Preparation (UNIMMAP) formulation10,19,20

Micronutrient |
Dose |
|---|---|
Vitamin A |
800µg |
Vitamin D |
200 IU |
Vitamin E |
10mg |
Niacin |
18mg |
Folic-acid |
400µg (0.4mg) |
Vitamin B1 |
1.4mg |
Vitamin B2 |
1.4mg |
Vitamin B6 |
1.9mg |
Vitamin B12 |
2.6µg |
Vitamin C |
70mg |
Zinc |
15mg |
Iron |
30mg |
Selenium |
65µg |
Copper |
2mg |
Iodine |
150µg |
Table 2: The United Nations International
Multiple Micronutrient Antenatal Preparation
(UNIMMAP) formulation10,19,20
| Micronutrient | Dose |
|---|---|
| Vitamin A | 800µg |
| Vitamin D | 200 IU |
| Vitamin E | 10mg |
| Niacin | 18mg |
| Folic-acid | 400µg (0.4mg) |
| Vitamin B1 | 1.4mg |
| Vitamin B2 | 1.4mg |
| Vitamin B6 | 1.9mg |
| Vitamin B12 | 2.6µg |
| Vitamin C | 70mg |
| Zinc | 15mg |
| Iron | 30mg |
| Selenium | 65µg |
| Copper | 2mg |
| Iodine | 150µg |
Evidence-based efficacy for MMN supplementation
In a Cochrane review,4 prospective randomized controlled trials evaluating MMN supplementation with iron and folic acid during pregnancy and its effects on the pregnancy outcome were evaluated. Results showed that pregnant women who received MMN supplementation had fewer LBW and SGA babies. Findings from another recently conducted Cochrane review10 suggest a positive impact of MMN supplementation with iron and folic acid on several birth outcomes. MMN supplementation in pregnancy led to a reduction in babies considered LBW, and a likely reduction in babies considered SGA, and preterm births.
In a double-blind cluster-randomised trial,22 it was observed that infants of women consuming MMN supplements had an 18% reduction in early infant mortality compared with those of women given iron and folic acid. Combined fetal loss and neonatal deaths were reduced by 11%. There was also a 14% decreased risk of LBW for those in the MMN group.
Evidence-based efficacy for MMN supplementation
In a Cochrane review,4 prospective randomized controlled trials evaluating MMN supplementation with iron and folic acid during pregnancy and its effects on the pregnancy outcome were evaluated. Results showed that pregnant women who received MMN supplementation had fewer LBW and SGA babies. Findings from another recently conducted Cochrane review10 suggest a positive impact of MMN supplementation with iron and folic acid on several birth outcomes. MMN supplementation in pregnancy led to a reduction in babies considered LBW, and a likely reduction in babies considered SGA, and preterm births.
In a double-blind cluster-randomised trial,22 it was observed that infants of women consuming MMN supplements had an 18% reduction in early infant mortality compared with those of women given iron and folic acid. Combined fetal loss and neonatal deaths were reduced by 11%. There was also a 14% decreased risk of LBW for those in the MMN group.
How to correct MMN deficiency in pregnancy?
A daily prenatal multivitamin is generally recommended before conception and during pregnancy.16 However, the problem of hidden hunger, coupled with an increased prevalence of MMN deficiency and associated adverse pregnancy outcomes, underscore the need to provide MMN supplementations rather than single preparations during the perinatal period to ensure smooth and successful pregnancy outcomes.17 In fact, combining different micronutrients necessary for pregnancy into one supplement has been suggested as a cost-effective way to achieve multiple benefits for women during pregnancy.10,12
The WHO at present recommends providing MMN supplements to pregnant women from populations with a high prevalence of maternal nutritional deficiencies, thus reducing the risks of LBW and small for gestational age (SGA) compared to iron-folic acid supplementation alone.18 The evidence derives from trials using the widely available United Nations International Multiple Micronutrient Antenatal Preparation (UNIMMAP), which contains 15 micronutrients including 10 vitamins and 5 minerals (Table 2).10,19,20 The MMN supplement based on the UNIMMAP formula provides women and their offspring with a healthy start to life in an efficacious, safe, and cost-effective way.21
References
1. Soma-Pillay P, Nelson-Piercy C, Tolppanen H, et al. Physiological changes in pregnancy. Cardiovasc J Afr. 2016;27(2):89-94. 2. Gómez MF, Field CJ, Olstad DL,et al; APrON Study Team. Use of micronutrient supplements among pregnant women in Alberta: results from the Alberta Pregnancy Outcomes and Nutrition (APrON) cohort. Matern Child Nutr. 2015;11(4):497-510. 3. Mousa A, Naqash A, Lim S. Macronutrient and Micronutrient Intake during Pregnancy: An Overview of Recent Evidence. Nutrients. 2019;11(2):443. 4. Beluska-Turkan K, Korczak R, Hartell B, et al. Nutritional Gaps and Supplementation in the First 1000 Days. Nutrients. 2019;11(12):2891. 5. Introductory Chapter: Impact of First 1000 Days Nutrition on Child Development and General Health. Available at: https://www.intechopen. com/chapters/73181. Accessed on 09/06/2022. 6. Hidden Hunger: The Irony of a Full Belly. Available at: http://agrpartners.com/wp-content/uploads/2013/08/ AGR-Thought-Piece-Hidden-Hunger.pdf. Accessed on 09/06/2022. 7. Lowe NM. The global challenge of hidden hunger: perspectives from the field. Proc Nutr Soc. 2021;80(3):283-289. 8. Ladipo OA. Nutrition in pregnancy: mineral and vitamin supplements. Am J ClinNutr. 2000;72(1 Suppl):280S-290S. 9. Gernand AD, Schulze KJ, Stewart CP, et al. Micronutrient deficiencies in pregnancy worldwide: health effects and prevention. Nat Rev Endocrinol. 2016;12(5):274-289. 10. Keats EC, Haider BA, Tam E, et al. Multiple-micronutrient supplementation for women during pregnancy. Cochrane Database Syst Rev. 2019;3(3):CD004905. 11. Toteja GS, Singh P, Dhillon BS, et al. Prevalence of anemia among pregnant women and adolescent girls in 16 districts of India. Food Nutr Bull. 2006;27(4):311-5. 12. Composition of a multi-micronutrient supplement to be used in pilot programmes among pregnant women in developing countries. Available at: https://apps.who.int/iris/ bitstream/handle/10665/75358/UNICEF-WHO-multi-micronutrients.pdf?sequence=1&isAllowed=y. Accessed on 09/06/2022. 13. Maheshwari KU, Kumar NA, Preethi S. Assessment of serum zinc levels among rural pregnant women in Chengalpettu district, Tamil Nadu. Int J Clin Biochem Res. 2020;7(3):320-324. 14. Radhika MS, Bhaskaram P, Balakrishna N, et al. Effects of vitamin A deficiency during pregnancy on maternal and child health. BJOG. 2002;109(6):689-93.15. Jeyakumar A, Shinde V, Ravindran R. Pooled estimate of vitamin D deficiency among pregnant women in India: a systematic review and meta-analysis. J Health Popul Nutr. 2021; 40:28. 16. Kominiarek MA, Rajan P. Nutrition Recommendations in Pregnancy and Lactation. Med Clin North Am. 2016;100(6):1199-1215. 17. Ramachandran V, Kanagasabai K, Kamaraj P, et al. Hidden Hunger (Micro Nutrient Deficiencies – MNDs) Among Pregnant Women and Pregnancy Outcomes. – A Hospital Based Study in Chennai. Int J Adv Res Biol Sci. 2015;2(12):100-111. 18. Parisi F, di Bartolo I, Savasi VM, et al. Micronutrient supplementation in pregnancy: Who, what and how much?. Obstet Med. 2019;12(1):5-13. 19. Tuncalp Ö, Rogers LM, Lawrie TA, et al. WHO recommendations on antenatal nutrition: an update on multiple micronutrient supplements. BMJ Glob Health. 2020;5(7):e003375. 20. WHO antenatal care recommendations for a positive pregnancy experience Nutritional interventions update: Multiple micronutrient supplements during pregnancy. Available at: https://apps.who.int/iris/rest/bitstreams/1289394/retrieve. Accessed on 10/06/2022. 21. Multiple Micronutrient Supplement Technical Advisory Group (MMS-TAG); Micronutrient Forum (MNF). Expert consensus on an open-access United Nations International Multiple Micronutrient Antenatal Preparation-multiple micronutrient supplement product specification. Ann N Y Acad Sci. 2020;1470(1):3-13. 22. The Supplementation with Multiple Micronutrients Intervention Trial (SUMMIT) Study Group. Effect of maternal multiple micronutrient supplementation on fetal loss and infant death in Indonesia: a double-blind cluster-randomised trial. The Lancet. 2008; 371(9608):215-227.