
|
DR. M. GOURI DEVI |
Immed. Past President, Indian Fertility Society |

DR. M. GOURI DEVI
MBBS, MD (Gynecology and Obstetrics)
Immed. Past President, Indian Fertility Society
Director, Ridge Fertility and IVF Group
Director, Gouri Hospital
Director, Ridge Healthcare
Executive, AOGD
Executive member, NARCHI
Multi-micronutrients supplementation and fertility
> Multi‐micronutrient (MMN) deficiencies often coexist among women of reproductive age in developing nations. Micronutrients exert beneficial effects on female fertility and play essential role in different stages of conception. Combining multiple micronutrients into one supplement has been proposed as a cost‐effective way to achieve multiple benefits for women during pregnancy1-3..
> Studies using MMN supplementation have demonstrated positive results on fertility in healthy women and in those already having problems conceiving (Box 1)1,2..
Box 1: Favorable effect of MMN supplementation on female fertility1,2
> Normalize trace element levels.
> Positive impact on the quality of the microfollicular environment.
> Positive effect on oocyte and embryo quality.
> Positive effect on implantation and live birth.
> Reduces the incidence of low birth weight, smallfor-gestational age, and preterm birth.
MMN supplementation improves IVF outcomes
> MMN supplementation in women during invitro fertilization (IVF) therapy has been shown to normalize trace element levels. This may exert a positive impact on the quality of the microfollicular environment, and thus on oocyte and embryo quality, implantation, and live birth (Box 1).1,2.
> Accumulating evidence suggests the importance of MMN supplementation in improving fertility in couples undergoing IVF therapy.4
> Arhin and colleagues4 conducted a systematic review of clinical evidences on the effect of micronutrients on primary outcome parameters of IVF treatment. A total of five studies were included that reported outcomes in 467 participants who were administered micronutrient supplements alone or in combination with other nutrients as part of IVF therapy.
> The results revealed a positive impact of MMN supplementation on clinical outcomes of IVF therapy in terms of pregnancy rate and/or live birth rate. The study authors concluded that MMN supplementation appears to influence positive outcomes in couples undergoing IVF treatment. MMN supplementations for IVF couples may prove to be a promising approach to improving IVF clinical outcomes.4
Multi-micronutrients supplementation and fertility
> Multi‐micronutrient (MMN) deficiencies often coexist among women of reproductive age in developing nations. Micronutrients exert beneficial effects on female fertility and play essential role in different stages of conception. Combining multiple micronutrients into one supplement has been proposed as a cost‐effective way to achieve multiple benefits for women during pregnancy1-3..
> Studies using MMN supplementation have demonstrated positive results on fertility in healthy women and in those already having problems conceiving (Box 1)1,2..
Box 1: Favorable effect of MMN supplementation on female fertility1,2
> Normalize trace element levels.
> Positive impact on the quality of the microfollicular environment.
> Positive effect on oocyte and embryo quality.
> Positive effect on implantation and live birth.
> Reduces the incidence of low birth weight, smallfor-gestational age, and preterm birth.
MMN supplementation improves IVF outcomes
> MMN supplementation in women during invitro fertilization (IVF) therapy has been shown to normalize trace element levels. This may exert a positive impact on the quality of the microfollicular environment, and thus on oocyte and embryo quality, implantation, and live birth (Box 1).1,2.
> Accumulating evidence suggests the importance of MMN supplementation in improving fertility in couples undergoing IVF therapy.4
> Arhin and colleagues4 conducted a systematic review of clinical evidences on the effect of micronutrients on primary outcome parameters of IVF treatment. A total of five studies were included that reported outcomes in 467 participants who were administered micronutrient supplements alone or in combination with other nutrients as part of IVF therapy.
> The results revealed a positive impact of MMN supplementation on clinical outcomes of IVF therapy in terms of pregnancy rate and/or live birth rate. The study authors concluded that MMN supplementation appears to influence positive outcomes in couples undergoing IVF treatment. MMN supplementations for IVF couples may prove to be a promising approach to improving IVF clinical outcomes.4
MMN impact on antioxidant defenses, oxidative stress, and fertility
> An open pilot study5 conducted to explore the effects of MMN supplementation on levels of oxidative stress and subsequent outcomes of IVF in women aged >39years demonstrated that MMN supplementation before IVF cycles significantly increased the total antioxidant capacity in serum and follicular fluid and protected proteins against oxidative damage compared with untreated controls.
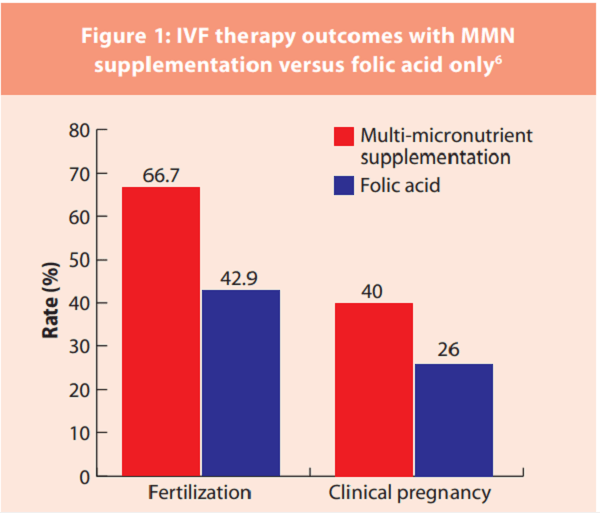
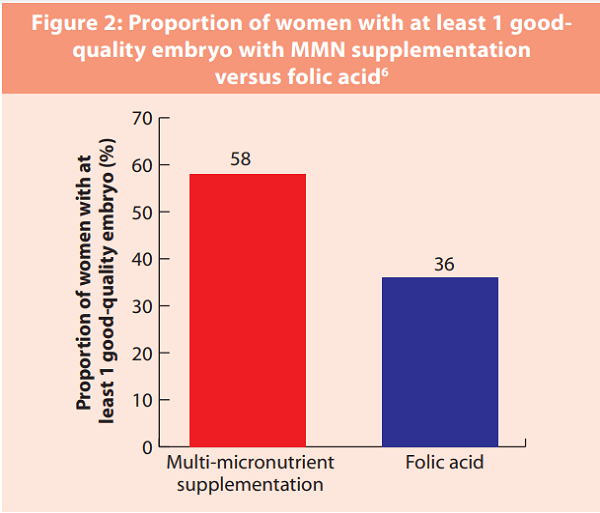
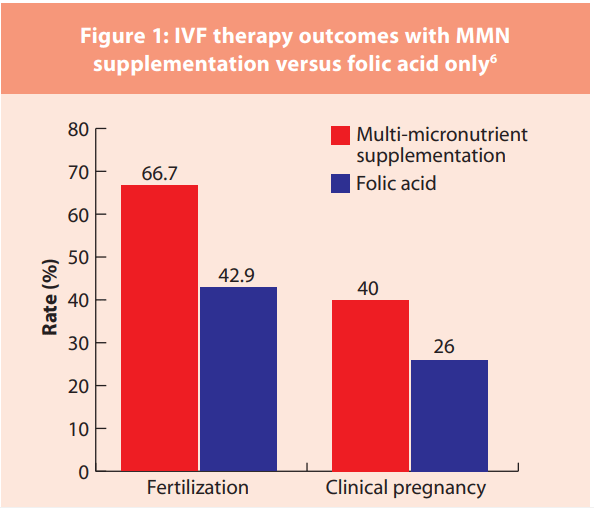
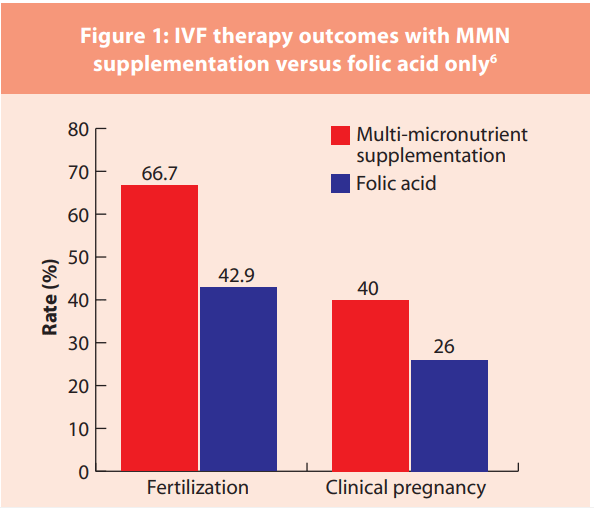
> Nouri K, et al6 conducted a prospective study to explore the effect of MMN supplementation on outcomes following IVF/intracytoplasmic sperm injection (ICSI). A total of 100 women undergoing IVF/ICSI were randomly assigned 1:1 to receive either MMN supplementation or 400 µg folic acid.
> Findings of this study suggested that MMN supplementation for a minimum of 28 days prior to ovarian hyperstimulation seems beneficial in terms of fertilization rate and embryo quality. 6
MMN impact on the time to pregnancy and chances of becoming pregnant
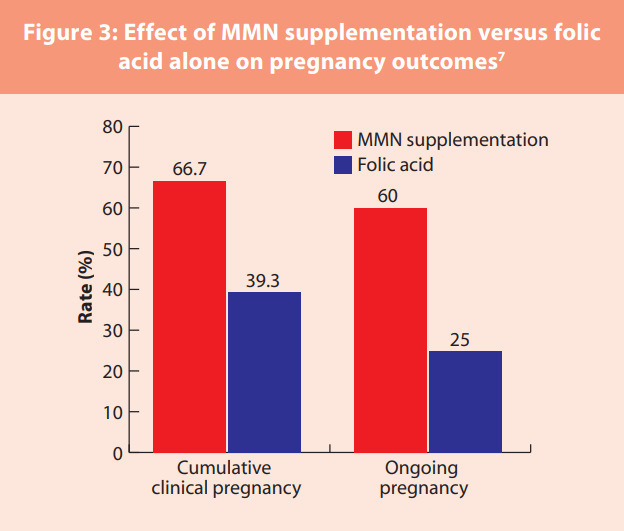
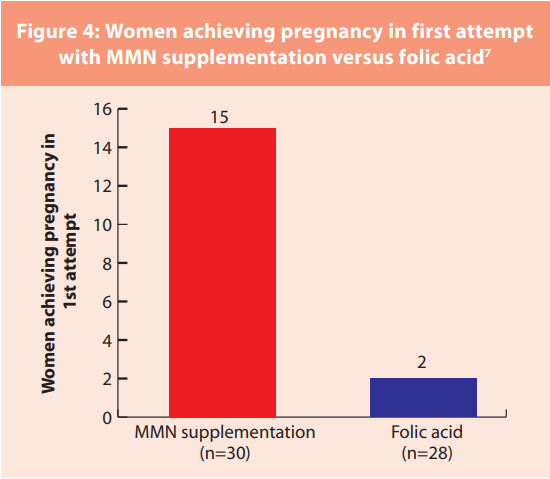
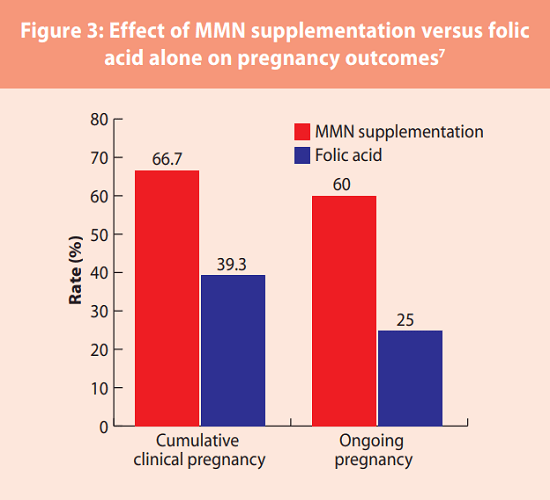
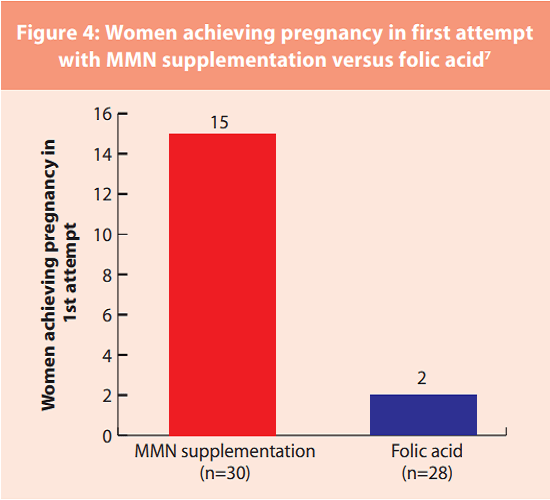
> Agrawal R, et al7 conducted a prospective randomized controlled trial to explore the effect of MMN supplementation versus folic acid alone on pregnancy outcomes in subfertile women undergoing ovulation induction using standard treatment regimens .
> A total of 58 women were allocated to either receive adjuvant MMN supplementation (n=30) or folic acid (n=28); 56 women completed the study (29 in the MMN group and 27 in the folic-acid group).
> The results revealed that the cumulative clinical pregnancy rate was significantly higher in the MMN group (66.7%) as compared with folic acid alone (39.3%). Likewise, the ongoing pregnancy rate was higher in the MMN group (60.0%) versus the folic-acid group (25.0%) (Figure 3). Moreover, significantly fewer attempts to achieve pregnancy were necessary in the MMN supplementation group compared with the folic-acid alone group (Figure 4).
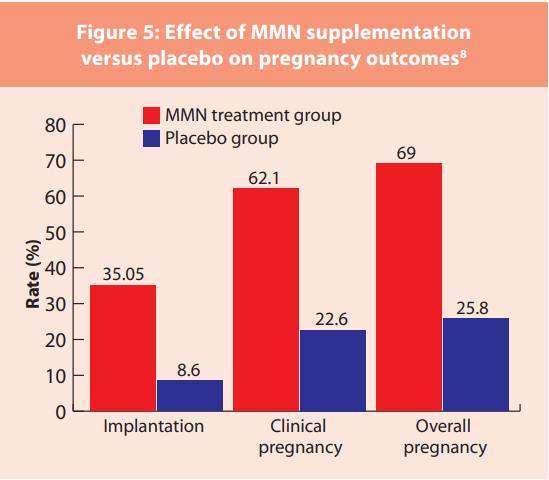
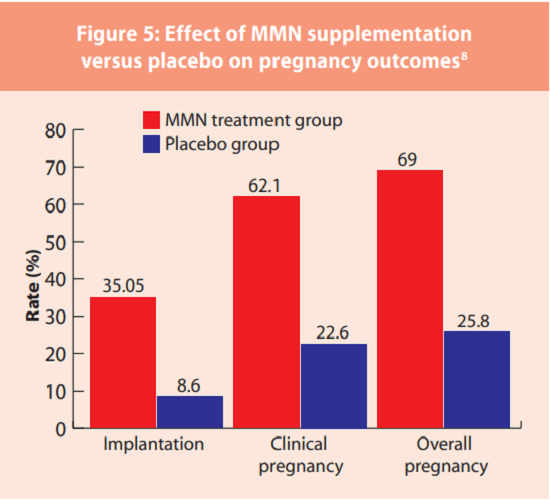
> Fatemi and colleagues,8 in a double-blinded randomized placebo-controlled trial, demonstrated that 8-week supplementation with MMN along with dietary counseling significantly improves clinical pregnancy in PCOS infertile women undergoing ICSI.
>Overall pregnancy rate and clinical pregnancy rate were significantly higher in the MMN treatment group compared to the placebo group. The MMN treatment group also had a significantly higher implantation rate (35.05%) as compared to the placebo group (8.6%) (Figure 5). Also, the treatment group had 20 successful deliveries as compared to 7 in the placebo group, which were monitored for one year confirming a healthy status.
> These results suggest that the use of ad-on MMN supplementation during ovulation induction provides greater odds of pregnancy compared with folic-acid alone.
MMN impact on antioxidant defenses, oxidative stress, and fertility
> An open pilot study5 conducted to explore the effects of MMN supplementation on levels of oxidative stress and subsequent outcomes of IVF in women aged >39years demonstrated that MMN supplementation before IVF cycles significantly increased the total antioxidant capacity in serum and follicular fluid and protected proteins against oxidative damage compared with untreated controls.
> Nouri K, et al6 conducted a prospective study to explore the effect of MMN supplementation on outcomes following IVF/intracytoplasmic sperm injection (ICSI). A total of 100 women undergoing IVF/ICSI were randomly assigned 1:1 to receive either MMN supplementation or 400 µg folic acid.
> Findings of this study suggested that MMN supplementation for a minimum of 28 days prior to ovarian hyperstimulation seems beneficial in terms of fertilization rate and embryo quality. 6
MMN impact on the time to pregnancy and chances of becoming pregnant
> Agrawal R, et al7 conducted a prospective randomized controlled trial to explore the effect of MMN supplementation versus folic acid alone on pregnancy outcomes in subfertile women undergoing ovulation induction using standard treatment regimens .
> A total of 58 women were allocated to either receive adjuvant MMN supplementation (n=30) or folic acid (n=28); 56 women completed the study (29 in the MMN group and 27 in the folic-acid group).
> The results revealed that the cumulative clinical pregnancy rate was significantly higher in the MMN group (66.7%) as compared with folic acid alone (39.3%). Likewise, the ongoing pregnancy rate was higher in the MMN group (60.0%) versus the folic-acid group (25.0%) (Figure 3). Moreover, significantly fewer attempts to achieve pregnancy were necessary in the MMN supplementation group compared with the folic-acid alone group (Figure 4).
> Fatemi and colleagues,8 in a double-blinded randomized placebo-controlled trial, demonstrated that 8-week supplementation with MMN along with dietary counseling significantly improves clinical pregnancy in PCOS infertile women undergoing ICSI.
>Overall pregnancy rate and clinical pregnancy rate were significantly higher in the MMN treatment group compared to the placebo group. The MMN treatment group also had a significantly higher implantation rate (35.05%) as compared to the placebo group (8.6%) (Figure 5). Also, the treatment group had 20 successful deliveries as compared to 7 in the placebo group, which were monitored for one year confirming a healthy status.
> These results suggest that the use of ad-on MMN supplementation during ovulation induction provides greater odds of pregnancy compared with folic-acid alone.
SUMMARY
> The first 1,000 days of fetal/infant life are considered the crucial periods in infant metabolic and cognitive development. It can be divided into three phases: the prenatal period; breast (or formula) feeding; and a period of increasing complementary feeding.9,10.
> Optimized nutrition during the first 1000 days is critical for healthy development and a healthy life for the newborn. Inadequate maternal nutrition during conception and pregnancy is associated with poor maternal and child health outcomes. MMN supplementation can minimise the risk of adverse pregnancy and birth outcomes by bridging the nutrient gaps for expectant mothers.11.12
> IVF therapy has been associated with an increased risk of adverse birth outcomes, such as 1.2–2 times the risk of preterm birth (PTB) and low birth weight (LBW), 1.2 times the risk of small for gestational age (SGA), and 1.5 times the risk of congenital abnormality.13,14
> In IVF therapy, preconception diet considerably affects reproductive outcomes including fertilization, embryo quality, and pregnancy complications .15
> Growing pool of evidence suggests that MMN supplementation may negate IVF-related adverse pregnancy outcomes including preeclampsia, LBW, SGA, preterm birth, and gestational diabetes mellitus .11
> A recent cohort study16 of women undergoing IVF found that pre-treatment intake of MMN including folate was associated with higher fertilization rates and decreased incidence of adverse pregnancy outcomes such as failed fertilization, implantation failure, and clinical pregnancy loss.
> Proper nutrition in the first 1,000 days ensures a higher likelihood of birthing at a healthy weight and a reduced risk of developing a number of illnesses and disorders.12
References
1. Keats EC, Haider BA, Tam E, et al. Multiple‐micronutrient supplementation for women during pregnancy. Cochrane Database of Systematic Reviews. 2019; 3: Art. No.: CD004905. 2. Schaefer E, Nock D. The Impact of Preconceptional Multiple-Micronutrient Supplementation on Female Fertility. Clin Med Insights Womens Health. 2019;12:1179562X19843868. 3. Kohil A, Chouliaras S, Alabduljabbar S, et al. Female infertility and diet, is there a role for a personalized nutritional approach in assisted reproductive technologies? A Narrative Review. Front Nutr. 2022;9:927972. 4. Arhin SK, Zhao Y, Lu X, et al. Effect of micronutrient supplementation on IVF outcomes: a systematic review of the literature. Reprod Biomed Online. 2017;35(6):715-722. 5. Luddi A, Capaldo A, Focarelli R, et al. Antioxidants reduce oxidative stress in follicular fluid of aged women undergoing IVF. Reprod Biol Endocrinol. 2016;14(1):57. 6. Nouri K, Walch K, Weghofer A, et al. The Impact of a Standardized Oral Multinutrient Supplementation on Embryo Quality in in vitro Fertilization/ Intracytoplasmic Sperm Injection: A Prospective Randomized Trial. Gynecol Obstet Invest. 2017;82(1):8-14. 7. Agrawal R, Burt E, Gallagher AM, et al. Prospective randomized trial of multiple micronutrients in subfertile women undergoing ovulation induction: a pilot study. Reprod Biomed Online. 2012;24(1):54-60. 8. Fatemi F, Mohammadzadeh A, Sadeghi MR, et al. Role of vitamin E and D3 supplementation in Intra-Cytoplasmic Sperm Injection outcomes of women with polycystic ovarian syndrome: A double blinded randomized placebo-controlled trial. Clin Nutr ESPEN. 2017;18:23-30. 9. Neville MC, Anderson SM, McManaman JL, et al. Lactation and neonatal nutrition: defining and refining the critical questions. J Mammary Gland Biol Neoplasia. 2012;17(2):167-88. 10. Mameli C, Mazzantini S, Zuccotti GV. Nutrition in the First 1000 Days: The Origin of Childhood Obesity. Int J Environ Res Public Health. 2016;13(9):838. 11. Beluska-Turkan K, Korczak R, Hartell B, et al. Nutritional Gaps and Supplementation in the First 1000 Days. Nutrients. 2019;11(12):2891. 12. Likhar A, Patil MS. Importance of Maternal Nutrition in the First 1,000 Days of Life and Its Effects on Child Development: A Narrative Review. Cureus. 2022;14(10):e30083. 13. Nagata C, Yang L, Yamamoto-Hanada K, et al; Japan Environment & Children’s Study Group. Complications and adverse outcomes in pregnancy and childbirth among women who conceived by assisted reproductive technologies: A nationwide birth cohort study of Japan environment and children’s study. BMC Pregnancy Childbirth. 2019;19(1):77. 14.Yu H, Liang Z, Cai R, et al. Association of adverse birth outcomes with in vitro fertilization after controlling infertility factors based on a singleton live birth cohort. Sci Rep. 2022;12(1):4528.15. Wu S, Zhang X, Zhao X, et al. Preconception Dietary Patterns and Associations With IVF Outcomes: An Ongoing Prospective Cohort Study. Front Nutr. 2022;9:808355. 16. Gaskins AJ, Toth TL, Chavarro JE. Prepregnancy Nutrition and Early Pregnancy Outcomes. Curr Nutr Rep. 2015;4(3):265-272.