|
Dr Sadhana Gupta |
NIGF, President – 2022-24 |

Dr Sadhana Gupta
Co chair Non Communicable disease committee of SAFOG
(South Asian Fed of ob Gyn)
NIGF, President – 2022-24
VICE PRESIDENT FOGSI 2016
ICOG Governing Council Member (2015-21)
chairperson fogsi safe motherhood committee
SENIOR OB Gyn JJ hospital Gorakhpur (India)
Secret of national health lies in the homes of the people
Hippocrates says 2500 year ago – “Let Food be thy medicine and medicine be thy food”. Around 1/10th of world population
is suffering from hidden hunger and 1/4th from evident nutritional deficiency. Women of reproductive age, pregnant and
lactating mothers are vulnerable section for nutritional deficiencies
Introduction
Nutrition is central to Sustainable Developmental Goal (SDG) agenda eliminating hunger and poverty is its aim. Equity and
equal opportunity for all is pathway to achieve substantiable developmental goal. At least 12 out of 17 SDG include indicators
for nutrition. Investing in actions to accelerate all forms of malnutrition is therefore critical to support achievement of country and global health targets.1
Intergenerational heritage of nutritional deficiencies in developing world
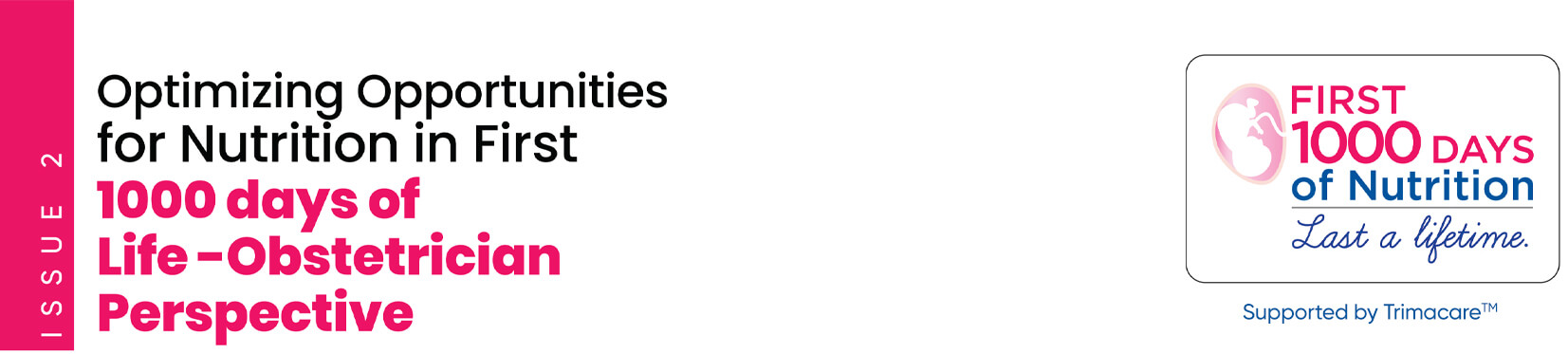
Deficiency of micronutrients are inherited across the generations. There is an intergenerational self-perpetuating cycle of anaemia & multi-micronutrient (MMN) deficiency in Indian population. Poor iron store at birth leads to low iron content of breast milk, added by low diet intake in infancy and childhood, aggravated due to increased requirement in adolescent, worsen during pregnancy and vicious cycle of low iron store at birth.(Fig.1: A, B)
Decreased resistance to infection due to immunodeficiency in pregnancy can lead to IUGR, preterm labor, low birth weight, low iron and multiple micronutrient deficiency. Multiple micro and macro nutrient deficiency leads to adverse obstetric outcome and increased maternal and neonatal morbidity and ortality.2
Secret of national health lies in the homes of the people
Hippocrates says 2500 year ago – “Let Food be thy medicine and medicine be thy food”. Around 1/10th of world population is suffering from hidden hunger and 1/4th from evident nutritional deficiency. Women of reproductive age, pregnant and lactating mothers are vulnerable section for nutritional deficiencies
Introduction
Nutrition is central to Sustainable Developmental Goal (SDG) agenda eliminating hunger and poverty is its aim. Equity and equal opportunity for all is pathway to achieve substantiable developmental goal. At least 12 out of 17 SDG include indicators for nutrition. Investing in actions to accelerate all forms of malnutrition is therefore critical to support achievement of country and global health targets.1
Intergenerational heritage of nutritional deficiencies in developing world
Deficiency of micronutrients are inherited across the generations. There is an intergenerational self-perpetuating cycle of anaemia & multi- icronutrient (MMN) deficiency in Indian population. Poor iron store at birth leads to low iron content of breast milk, added by low diet intake in infancy and childhood, aggravated due to increased requirement in adolescent, worsen during pregnancy and vicious cycle of low iron store at birth. (Fig.1: A, B)
Decreased resistance to infection due to immunodeficiency in pregnancy can lead to IUGR, preterm labor, low birth weight, low iron and ultiple micronutrient deficiency. Multiple micro and macro nutrient deficiency leads to adverse obstetric outcome and increased maternal and neonatal morbidity and mortality2
Concept of First 1000 days of Nutrition
Nutrition during first 1000 days of child’s life gives a critical window of opportunity hich has great impact on short and long-term health of mother and next eneration. Fetal origin of adult disease explains and emphasize correct nutrition in utero to prevent future health complications in neonate and adults.3 Currently when developing countries are struggling with high incidence of non-communicable disease, awareness of obstetric care provider about correct nutritional intervention will play a great role in making India healthy in next decades
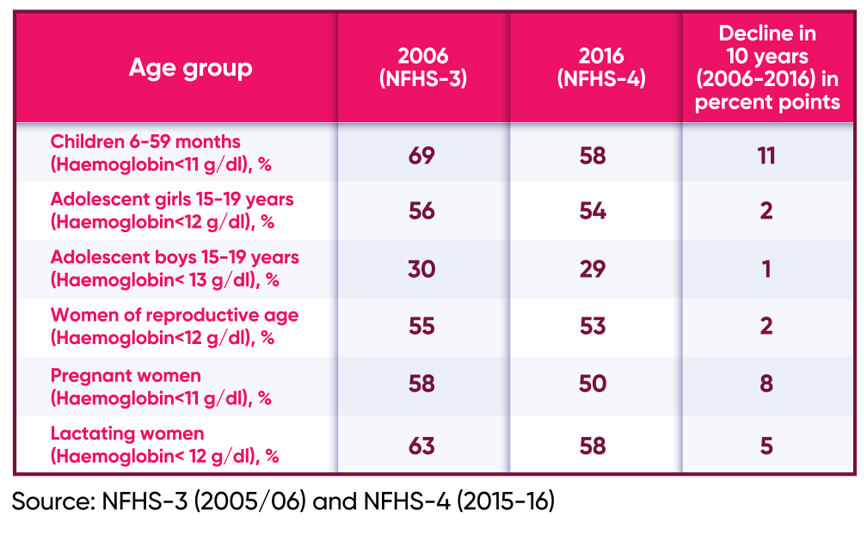
India carries the largest burden of Anaemia globally. Progress to reduce Anaemia has been slow and uneven despite substantial economic growth and 50 years of programmatic effort. (Box 1) Micronutrient deficiencies are considered one of the crucial factors in our slow achievement in reduction of anemia in general and pregnant population.
Box 1: Summarizes incidence of anemia in different age groups
 Micronutrients Deficiencies –Hidden Hunger
Micronutrients Deficiencies –Hidden Hunger
Micronutrient deficiencies are determining and aggravating factors for health status and quality of life. Hidden hunger impairs physical growth and learning, limits productivity and ultimately perpetuates poverty in a continues cycle. Multiple micronutrient (MMN) deficiencies is one of the important cause of missing the targets for reducing anemia in pregnant women and women of reproductive age in India despite a long history of public health program of providing iron and folic acid to pregnant women. Physical and cognitive loss due to Anemia cost the developing countries up to 4.5% loss in GDP er annum which is 1.18 % of GDP in India, thereby stalling social and economic development.4
It is time to see and act beyond conventional iron and folic acid supplementation. Besides opportunity and equality gaps remains which need to be filled. It is critical to bridge these opportunity and equality gaps by addressing policy and programmatic delivery systems bottle necks to achieve universal coverage for both health and nutrition within delivery system.1
Obstetrician Perspective
Pregnancy is time of rapid and profound physiological changes from the time of conception until birth. Nutritional requirement increases during pregnancy to maintain maternal metabolism and tissue accretion while supporting fetal growth and development Poor dietary intake or deficiency in key macro and micro nutrient can therefore have substantial impact on pregnancy outcome and neonatal health. Although a healthy and varied diet remains the preferred means of meeting nutritional requirement, some nutritional needs in pregnancy are challenging to meet with diet alone. Obstetrician have unique opportunity to intervention for healthy nutrition in form of nutritional education, prescribing right nutrient and individualizing diet and nutrition as per women clinical profile. Besides from first to third trimester requirement of mother and fetus changes. In first trimester there is fetal organogenesis while in second and third trimester fetus gains weight and organs are matured. Fetal brain development and cognitive function depends on many micronutrients, traceelements and DHA especially in late second trimester and third trimester
Consideration of Gestation specific Nutritional Supplementation is one of the paradigms shifts in Antenatal care
Folic acid and micronutrient -Any women considering pregnancy should take 200 µg + a folate supplement containing 400 µg. Pregnancy is associated with increased folate demand due to growth of fetus and uteroplacental organ, rapid plasma clearance by increased catabolism and urinary folate excretion. Folic acid supplementation in pre and early conception reduces fetal Neural Tube efect as well other fetal birth defect.Besides it reduces homocysteine level hich reduces incidence of adverse obstetric outcome. In high-risk regnancies MethylTHF is better alternative due to widely prevalent genetic polymorphism in various enzymes. Supplementation of the natural form,5-MethylTHF, is a better alternative to supplementation of FA, especially in countries not applying a fortification program.5
Hyper Homocysteinemia & Multiple Micronutrient
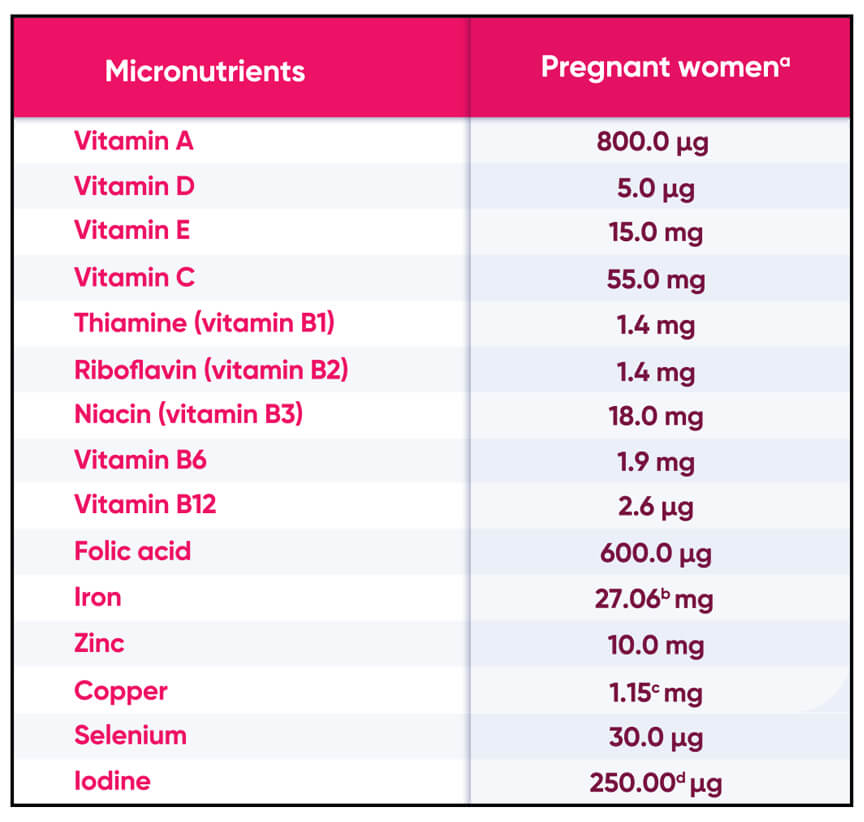
The vitamins, folate and cobalamin are involved in the re-methylation of homocysteine into methionine one can be metabolism. Vitamin B 6 as Pyridoxal 5 phosphate is a cofactor in trans sulphuration of homocysteine by way of cystathione to cysteine. A shortage of these vitamins, increased age and polymorphism in related enzymes lead to elevated homocysteine plasma concentration. Hyperhomocysteinemia has been directly corelated with vascular pregnancy complications like early pregnancy loss, placental abruptio and preeclampsia, IUGR, birth defects and preterm labor. Requirement of multi micronutrients in pregnancy is shown in Box-2
Box 2: Summarizes Vitamin requirement in Pregnancy
FOGSI 2017 GCPR strongly recommends Multiple micronutrient supplementation in pregnancy. All Women of reproductive age should be encouraged to take a folic acid containing multivitamin supplement for purpose of supporting healthy pregnancy outcome and prevent congenital anomalies — Strong Recommendation A, Quality evidence – 11 FOGSI GCPR
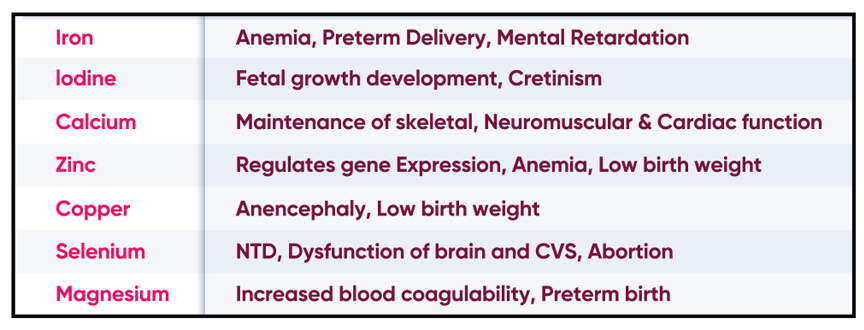
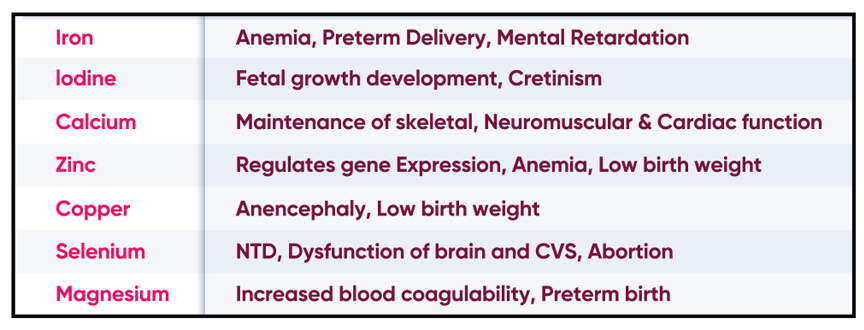
Trace elements in Pregnancy
Box 3: ummarizes function of various trace elements in fetal development and maternal ealth
<!–
Key points
–>
.fieldcss {border: 6px solid #b60057 !important; box-sizing: border-box; grid-area: 1 / 1; padding: 20px;width: inherit;border-radius: 25px !important;}.legcss{text-align: center;padding: 20px;background: #b60057;border: 2px solid #fff; border-radius: 37px; color: #fff; font-size: 36px;}
References
Ref. 1: Phuong Hong Nguyen et aal, BMJ global health 2021
Ref. 2: K.Kalaivani, Indian Jr. of Medical Research 2009
Ref. 3: Anderson et al 2001, Prac Nutr
Ref. 4: Klai et al 2011, Alhalaki et al 2016, Mantovani et al 2014 Indrani mukhopadhyay et al 2017
Ref. 5: J Perinat Med. 2013 Sep 1;41(5):469-83. Doi: 10.1515/jpm-2012-0256
Ref. 6: Syst. review 2019 WHO 2018
Concept of First 1000 days of Nutrition
Nutrition during first 1000 days of child’s life gives a critical window of opportunity which has great impact on shortand long-term health of mother and next generation. Fetal origin of adult disease explains and emphasize correct nutrition in utero to prevent future health complications in neonate and adults.3 Currently when developing countries are struggling with high incidence of non-communicable disease, awareness of obstetric care provider about correct nutritional intervention will play a great role in making India healthy in next decades India carries the largest burden of Anaemia globally. Progress to reduce Anaemia has been slow and uneven despite substantial economic growth and 50 years of programmatic effort. (Box 1) Micronutrient deficiencies are considered one of the crucial factors in our slow achievement in reduction of anemia in general and pregnant population.
Box 1: Summarizes incidence of anemia in different age groups
Micronutrients Deficiencies – Hidden Hunger
Micronutrient deficiencies are determining and aggravating factors for health status and quality of life. Hidden hunger impairs physical growth and learning, limits productivity and ultimately perpetuates poverty in a continues cycle. Multiple micronutrient (MMN) deficiencies is one of the important cause of missing the targets for reducing anemia in pregnant women and women of reproductive age in India despite a long history of public health program of providing iron and folic acid to pregnant women. Physical and cognitive loss due to Anemia cost the developing countries up to 4.5 % loss in GDP per annum which is 1.18 % of GDP in India, thereby stalling social and economic development.4 It is time to see and act beyond conventional iron and folic acid supplementation. Besides opportunity and equality gaps remains which need to be filled. It is critical to bridge these opportunity and equality gaps by addressing policy and programmatic delivery systems bottle necks to achieve universal coverage for both health and nutrition within delivery system.1
Obstetrician Perspective
Pregnancy is time of rapid and profound physiological changes from the time of conception until birth. Nutritional requirement increases during pregnancy to maintain maternal metabolism and tissue accretion while supporting fetal growth and evelopment. Poor dietary intake or deficiency in key macro and micro nutrient can therefore have substantial impact on pregnancy outcome and neonatal health. Although a healthy and varied diet remains the preferred means of meeting nutritional requirement, some nutritional needs in regnancy are challenging to meet with diet alone. Obstetrician have unique opportunity to intervention for healthy nutrition in form of nutritional education, prescribing right nutrient and individualizing diet and utrition as per women clinical profile. Besides from first to third rimester requirement of mother and fetus changes. In first trimester there is fetal organogenesis while in second and third trimester fetus gains weight and organs are matured. Fetal brain development and cognitive function depends on many micronutrients, traceelements and DHA especially in late second trimester and third trimester.
Consideration of Gestation specific Nutritional Supplementation is one of the paradigms shifts in Antenatal care
Folic acid and micronutrient -Any women considering pregnancy should take 200 µg + a folate supplement containing 400 µg. Pregnancy is associated with increased folate demand due to growth of fetus and uteroplacental organ, rapid plasma clearance by increased catabolism and urinary folate excretion. Folic acid supplementation in pre and early conception reduces fetal Neural Tube efect as well other fetal birth defect. Besides it reduces homocysteine level which reduces incidence of adverse obstetric outcome. In high-risk pregnancies MethylTHF is better alternative due to widely prevalent genetic polymorphism in various enzymes. Supplementation of the natural form,
5-methylTHF, is a better alternative to supplementation of FA, especially in countries not applying a fortification program.5
Hyper Homocysteinemia & Multiple Micronutrient
The vitamins, folate and cobalamin are involved in the re-methylation of homocysteine into methionine one can be metabolism. Vitamin B 6 as Pyridoxal 5 phosphate is a cofactor in trans sulphuration of homocysteine by way of cystathione to cysteine. A shortage of these vitamins, increased age and polymorphism in related enzymes lead to elevated homocysteine plasma concentration. Hyperhomocysteinemia has been directly corelated with vascular pregnancy complications like early pregnancy loss, placental abruptio and preeclampsia, IUGR, birth defects and preterm labor. Requirement of multi micronutrients in pregnancy is shown in Box-2
Box 1: Summarizes incidence of anemia in
different age groups.
FOGSI 2017 GCPR strongly recommends Multiple micronutrient supplementation in pregnancy. All Women of reproductive age should be encouraged to take a folic acid containing multivitamin supplement for purpose of supporting healthy pregnancy outcome and prevent congenital anomalies — Strong Recommendation A, Quality evidence – 11 FOGSI GCPR
Trace elements in Pregnancy
Box 3: ummarizes function of various trace elements in fetal development and maternal ealth
<!–
Key points
–>
.fieldcss {border: 6px solid #b60057 !important; box-sizing: border-box; grid-area: 1 / 1; padding: 11px;width: inherit;border-radius: 25px !important;}.legcss{text-align: center;padding: 11px;background: #b60057;border: 2px solid #fff; border-radius: 37px; color: #fff; font-size: 36px;}
References
Ref. 1: Phuong Hong Nguyen et aal, BMJ global health 2021
Ref. 2: K.Kalaivani, Indian Jr. of Medical Research 2009
Ref. 3: Anderson et al 2001, Prac Nutr
Ref. 4: Klai et al 2011, Alhalaki et al 2016, Mantovani et al 2014 Indrani mukhopadhyay et al 2017
Ref. 5: J Perinat Med. 2013 Sep 1;41(5):469-83. Doi: 10.1515/jpm-2012-0256
Ref. 6: Syst. review 2019 WHO 2018