|
Dr. Fessy Louis T |
Dept. of Reproductive Medicine & Surgery, |

Dr. Fessy Louis T
Senior Consultant & Associate Professor
Dept. of Reproductive Medicine & Surgery,
AIMS – AMRITA Institute of Medical Sciences, Kochi.
FOGSI All India Vice President 2021-22
ICOG- Governing Council Member
ISAR- National Executive Member
Obstetrician: The First Doctor of Life
As mentioned by Prof. CN Purandare, the past president of FIGO and a respected gynaecologist and obstetrician with more than 45 years of experience, “A Doctor’s life is a fascinating journey of several ups and downs, of feelings, making a difference in the lives of those
who have placed their precious lives in their hands.”1 In context, this becomes more stimulating for an obstetrician as he or she have to deal with the two lives i.e., of the baby and mother. Regardless of the child’s gender, it is the first encounter for her/him with a doctor who facilitates its journey and transition from the womb to the external world.
Nevertheless, the practice of an obstetrician is extremely demanding in a country like India where about 37,000 obstetricians need each single one to deliver or supervise average 800 deliveries; while it is well-known that anything > 200–300 per year deliveries can be a physical, mental and emotional nightmare for any for an obstetrician.1 This pressure often gets further compounded by the expectations of the would be parents. Yet, in the end it is extremely satisfying for most obstetricians caring for two lives at once; especially considering the fact that obstetric care offers a critical window of opportunity to facilitate and ensure happy outcomes for both the mother and the child in both short- and long-term. In this short review, we discuss about the need and importance of apposite nutrition during the “First 1000 days of life”
Relationship between your prenatal and adult life: “Barker hypothesis”
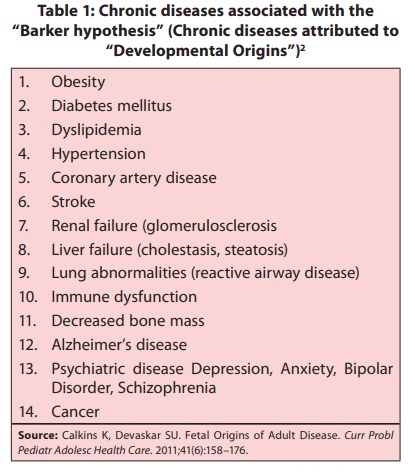
The “Barker hypothesis” is a near exact impression that provides a glimpse of the importance of early life care and well-being. Dr. David Barker first popularized the concept of “Fetal origins of adult disease (FOAD)”,also popularly known as the “Barker hypothesis”.2 Since its inception, the FOAD hypothesis has received considerable attention. It basically holds that events during early development of a child have a profound impact on his/her risk for development of future adult disease. Low birth weight, a surrogate marker of poor fetal growth and nutrition, and a proxy for intrauterine growth retardation (IUGR), is linked to various chronic diseases like coronary artery disease (CAD), hypertension, obesity, insulin resistance, and type 2 diabetes (Table 1).2,3 These relationships are further modified by patterns of postnatal growth; with “fetal developmental programming by nutritional stimuli” being one of the most widely accepted mechanisms thought to underlie these relationships.4,5.
Obstetrician: The First Doctor of Life
As mentioned by Prof. CN Purandare, the past president of FIGO and a respected gynaecologist and obstetrician with more than 45 years of experience, “A Doctor’s life is a fascinating journey of several ups and downs, of feelings, making a difference in the lives of those
who have placed their precious lives in their hands.”1 In context, this becomes more stimulating for an obstetrician as he or she have to deal with the two lives i.e., of the baby and mother. Regardless of the child’s gender, it is the first encounter for her/him with a doctor who facilitates its journey and transition from the womb to the external world.
Nevertheless, the practice of an obstetrician is extremely demanding in a country like India where about 37,000 obstetricians need each single one to deliver or supervise average 800 deliveries; while it is well-known that anything > 200–300 per year deliveries can be a physical, mental and emotional nightmare for any for an obstetrician.1 This pressure often gets further compounded by the expectations of the would be parents. Yet, in the end it is extremely satisfying for most obstetricians caring for two lives at once; especially considering the fact that obstetric care offers a critical window of opportunity to facilitate and ensure happy outcomes for both the mother and the child in both short- and long-term. In this short review, we discuss about the need and importance of apposite nutrition during the “First 1000 days of life”
Relationship between your prenatal and adult life: “Barker hypothesis”
The “Barker hypothesis” is a near exact impression that provides a glimpse of the importance of early life care and well-being. Dr. David Barker first popularized the concept of “Fetal origins of adult disease (FOAD)”, also popularly known as the “Barker hypothesis”.2 Since its inception, the FOAD hypothesis has received considerable attention. It basically holds that events during early development of a child have a profound impact on his/her risk for development of future adult disease. Low birth weight, a surrogate marker of poor fetal growth and nutrition, and a proxy for intrauterine growth retardation (IUGR), is linked to various chronic diseases like coronary artery disease (CAD), hypertension, obesity, insulin resistance, and type 2 diabetes (Table 1).2,3 These relationships are further modified by patterns of postnatal growth; with “fetal developmental programming by nutritional stimuli” being one of the most widely accepted mechanisms thought to underlie these relationships.4,5.
THE INDIAN GOVERNMENT HAS ALSO ACKNOWLEDGED THIS IMPORTANCE OF THE FIRST 1000 DAYS OF PREGNANCY, AND HAS SHIFTED THE FOCUS OF RASTRIYA BAL SWASHTHYA KARYAKRAM (RBSK) FROM “ONLY SURVIVAL TO HEALTHY SURVIVAL”
First 1000 Days of nutrition
As clearly reflected in the above discussion, prenatal nutrition lays the foundation for the development and health of the child not just during pregnancy, but for adulthood as well. Herein, in sequence to the prenatal nutrition, early postnatal nutrition is also vital determinant of adult health with significance rooted in the same construct of “developmental programming” even if partly; studies in this context support the contribution of postnatal nutrition and dietary composition and the rate of extrauterine growth to long-term metabolic outcomes and health.6,7
Amalgamation of both these aspects – prenatal and early postnatal nutrition – has given an inimitable concept in form of the “First 1000 Days of nutrition”, which is now globally recognized. According to this, the first 1000 days of child is a period of unique opportunity when the foundation of optimum health, growth and brain development across the lifespan are established. 8 fact, the Indian government has also acknowledged this importance of the first 1000 days of pregnancy, and has shifted the focus of Rastriya Bal Swashthya Karyakram (RBSK) from “only survival to healthy survival”.9
Not a full Plate: Limitations of current dietary patterns
While the concept of nutrition and its modulation for good health seems enticing, its application in the real-world is often challenging given the influence of several variables related both to the host and the environment. One such direct factor is the deficiencies of micronutrients in the diet. The effects of this micronutrient deficiency (hidden hunger) is detrimental to any person’s growth, immunity; nonetheless, the effects are particularly acute on the child’s health and survival, especially within the first 1,000 days of a child’s life, from conception to the age of two, resulting in serious physical and cognitive consequences.10-12 In fact, pregnant women and children are the primary victims of this hidden hunger.13
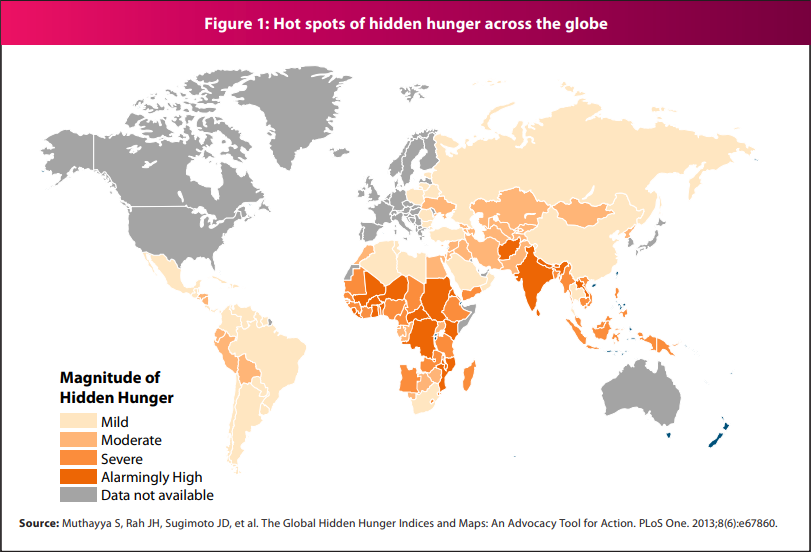
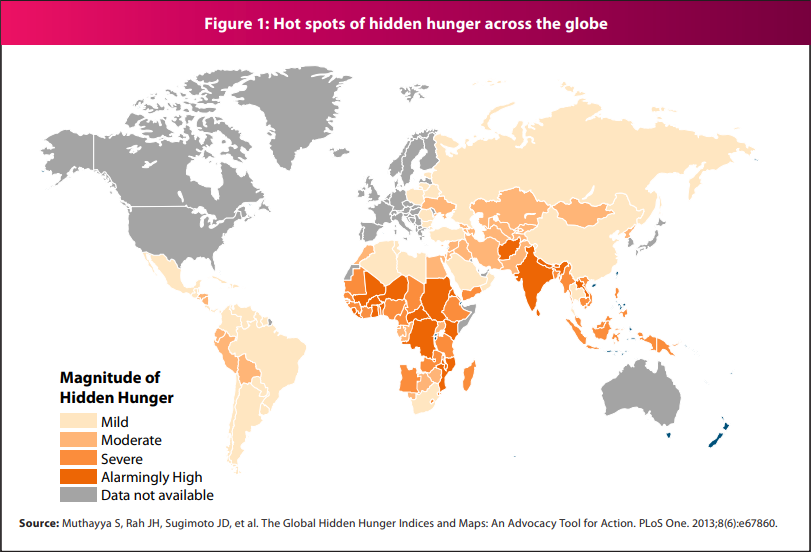
With a sweeping change in lifestyle and eating habits, pregnant women in low-resource settings (like India) now suffer from this common condition called “Hidden Hunger”, where they are eating sufficient food but are still under nourished. It is known that the quantity and quality of the world’s food supply varies from country to country, and even neighborhood to neighborhood; while some individuals face visible starvation, others consume high-calorie, high-fat meals that lack significant nutritional value, which in itself is a different form of starvation.2 This “nutritional transition” is not solely limited to India but has occurred on all continents. However, although global in scale, the prevalence of micronutrient deficiencies is particularly high in South Asia despite. In fact, India is one of the top nations with an alarmingly high level of hidden hunger (Figure 1).2,15,16 Pregnant women in India typically have diets characterized by low energy, macronutrient imbalance, and inadequate micronutrient intake. .17
Common nutritional practice being currently followed in pregnancy: Your IFC might not be sufficient
The most desirable approach to prevent micronutrient deficiencies in pregnancy is to assure a sustained diet of various micronutrient dense foods. However, this approach is often difficult to attain, and hence preventing adverse maternal and child outcomes due to micronutrient deficiencies through supplementation represents a sound and effective strategy.12 Further, it is important to note that the combination ingredients in the dietary supplement provide a wholesome approach to bridge the nutrition gap seen in pregnancy and early postnatal period. A recent analysis of the situation of maternal diets in India showed that intakes of essential micronutrients such as iron, vitamin A, riboflavin, vitamin C, and folic acid were less than 50% of RDA among most pregnant women in India.1.17
Several factors might contribute in this pattern of dietary insufficiency for the pregnant mothers, and one of them could be the availability of appropriate supplement combinations. Most of the supplements available in the market provide only a few nutrients recommended for pregnant women, which could be an influence of the health policy also even if partly. As part of antenatal care services in India, pregnant women receive iron, folic acid and calcium (IFC) only as micronutrient supplements.17 The IFC approach could be right at the macro level seeing the high population and low-resource status of the nation. However, at the same time it is critical to consider that besides IFC (Iron, Folate and calcium), other nutrients like iodine, Omega-3 fatty acids, Vitamin A, B and D are also important for the maternal and child health;18,19 and hence availability of varied combinations of nutrients in addition to those guided by the health policy should not be limitation. In addition, adherence to therapy is important to get the optimal benefits of the supplementation.
MMN supplementation during “first 1000 days of pregnancy”: A right approach recommended by WHO
It is now evident that multiple micronutrient (MMN) supplementation, that is, supplements providing several vitamins and minerals, can prove crucial for healthy pregnancy and better outcomes. In fact, most recent evidence validates this prospect that antenatal MMN supplements are more effective than iron and folic acid (IFA) supplements in reducing adverse pregnancy outcomes. MMN supplementation can fill the nutrient gaps for pregnant women and be a safe and cost‐effective intervention to reduce adverse pregnancy and birth outcomes. In fact, the recent 2020 WHO guidelines on the use of MMN supplementation during pregnancy recommended this intervention “in the context of rigorous research”; which was an update to the “not recommended” decision from the 2016 WHO guidelines, wherein daily use of IFA supplements was recommended.20 In fact, estimates from developing countries indicate that this policy change of replacing IFA supplements with MMN supplements would cost‐ effectively save lives and reduce the life‐long disabilities. Improvements in supplement adherence would be expected to further improve the cost‐effectiveness of replacing IFA with MMN supplements.21
Table 1: Chronic diseases associated with the “Barker hypothesis” (Chronic diseases attributed to “Developmental Origins”)2
THE INDIAN GOVERNMENT HAS ALSO ACKNOWLEDGED THIS IMPORTANCE OF THE FIRST 1000 DAYS OF PREGNANCY, AND HAS SHIFTED THE FOCUS OF RASTRIYA BAL SWASHTHYA KARYAKRAM (RBSK) FROM “ONLY SURVIVAL TO HEALTHY SURVIVAL”
First 1000 Days of nutrition
As clearly reflected in the above discussion, prenatal nutrition lays the foundation for the development and health of the child not just during pregnancy, but for adulthood as well. Herein, in sequence to the prenatal nutrition, early postnatal nutrition is also vital determinant of adult health with significance rooted in the same construct of “developmental programming” even if partly; studies in this context support the contribution of postnatal nutrition and dietary composition and the rate of extrauterine growth to long-term metabolic outcomes and health.6,7
Amalgamation of both these aspects – prenatal and early postnatal nutrition – has given an inimitable concept in form of the “First 1000 Days of nutrition”, which is now globally recognized. According to this, the first 1000 days of child is a period of unique opportunity when the foundation of optimum health, growth and brain development across the lifespan are established. 8 fact, the Indian government has also acknowledged this importance of the first 1000 days of pregnancy, and has shifted the focus of Rastriya Bal Swashthya Karyakram (RBSK) from “only survival to healthy survival”.9
Not a full Plate: Limitations of current dietary patterns
While the concept of nutrition and its modulation for good health seems enticing, its application in the real-world is often challenging given the influence of several variables related both to the host and the environment. One such direct factor is the deficiencies of micronutrients in the diet. The effects of this micronutrient deficiency (hidden hunger) is detrimental to any person’s growth, immunity; nonetheless, the effects are particularly acute on the child’s health and survival, especially within the first 1,000 days of a child’s life, from conception to the age of two, resulting in serious physical and cognitive consequences.10-12 In fact, pregnant women and children are the primary victims of this hidden hunger.13
With a sweeping change in lifestyle and eating habits, pregnant women in low-resource settings (like India) now suffer from this common condition called “Hidden Hunger”, where they are eating sufficient food but are still under nourished. It is known that the quantity and quality of the world’s food supply varies from country to country, and even neighborhood to neighborhood; while some individuals face visible starvation, others consume high-calorie, high-fat meals that lack significant nutritional value, which in itself is a different form of starvation.2 This “nutritional transition” is not solely limited to India but has occurred on all continents. However, although global in scale, the prevalence of micronutrient deficiencies is particularly high in South Asia despite. In fact, India is one of the top nations with an alarmingly high level of hidden hunger (Figure 1).2,15,16 Pregnant women in India typically have diets characterized by low energy, macronutrient imbalance, and inadequate micronutrient intake. .17
Common nutritional practice being currently followed in pregnancy: Your IFC might not be sufficient
The most desirable approach to prevent micronutrient deficiencies in pregnancy is to assure a sustained diet of various micronutrient dense foods. However, this approach is often difficult to attain, and hence preventing adverse maternal and child outcomes due to micronutrient deficiencies through supplementation represents a sound and effective strategy.12 Further, it is important to note that the combination ingredients in the dietary supplement provide a wholesome approach to bridge the nutrition gap seen in pregnancy and early postnatal period. A recent analysis of the situation of maternal diets in India showed that intakes of essential micronutrients such as iron, vitamin A, riboflavin, vitamin C, and folic acid were less than 50% of RDA among most pregnant women in India.1.17
Several factors might contribute in this pattern of dietary insufficiency for the pregnant mothers, and one of them could be the availability of appropriate supplement combinations. Most of the supplements available in the market provide only a few nutrients recommended for pregnant women, which could be an influence of the health policy also even if partly. As part of antenatal care services in India, pregnant women receive iron, folic acid and calcium (IFC) only as micronutrient supplements.17The IFC approach could be right at the macro level seeing the high population and low-resource status of the nation. However, at the same time it is critical to consider that besides IFC (Iron, Folate and calcium), other nutrients like iodine, Omega-3 fatty acids, Vitamin A, B and D are also important for the maternal and child health;18,19and hence availability of varied combinations of nutrients in addition to those guided by the health policy should not be limitation. In addition, adherence to therapy is important to get the optimal benefits of the supplementation.
MMN supplementation during “first 1000 days of pregnancy”: A right approach recommended by WHO
It is now evident that multiple micronutrient (MMN) supplementation, that is, supplements providing several vitamins and minerals, can prove crucial for healthy pregnancy and better outcomes. In fact, most recent evidence validates this prospect that antenatal MMN supplements are more effective than iron and folic acid (IFA) supplements in reducing adverse pregnancy outcomes. MMN supplementation can fill the nutrient gaps for pregnant women and be a safe and cost‐effective intervention to reduce adverse pregnancy and birth outcomes. In fact, the recent 2020 WHO guidelines on the use of MMN supplementation during pregnancy recommended this intervention “in the context of rigorous research”; which was an update to the “not recommended” decision from the 2016 WHO guidelines, wherein daily use of IFA supplements was recommended.20 In fact, estimates from developing countries indicate that this policy change of replacing IFA supplements with MMN supplements would cost‐ effectively save lives and reduce the life‐long disabilities. Improvements in supplement adherence would be expected to further improve the cost‐effectiveness of replacing IFA with MMN supplements.21
.fieldcss{border:6px solid #b60057!important;box-sizing:border-box;grid-area:1/1;padding:20px;width:inherit;border-radius:25px!important}.legcss{text-align:center;padding:20px;background:#b60057;border:2px solid #fff;border-radius:37px;color:#fff;font-size:36px}
References
1. Purandare CN. Life of an Obstetrician and Gynaecologist: A 45 Years Journey. The Journal of Obstetrics and Gynecology of India (May-June 2020);70(3):181–183. 2. Calkins K, Devaskar SU. Fetal Origins of Adult Disease. Curr Probl Pediatr Adolesc Health Care. 2011;41(6):158–176. 3. Zanetti D, Tikkanen E, Gustafsson S. Birthweight, Type 2 Diabetes Mellitus, and Cardiovascular Disease: Addressing the Barker Hypothesis With Mendelian Randomization. Circ Genom Precis Med. 2018;11(6):e002054. 4. A de Boo H, Harding JE. The developmental origins of adult disease (Barker) hypothesis. Aust N Z J Obstet Gynaecol. 2006;46(1):4-14. 5. Marousez L, Lesage J, Eberlé D. Epigenetics: Linking Early Postnatal Nutrition to Obesity Programming? Nutrients. 2019;11(12):2966. 6. Wiedmeier JE, Joss-Moore LA, Lane RH. Early postnatal nutrition and programming of the preterm neonate. Nutr Rev. 2011;69(2):76-82. 7. Neu J, Hauser N, Douglas-Escobar M. Postnatal nutrition and adult health programming. Semin Fetal Neonatal Med. 2007;12(1):78-86. 8. Cusick S, Georgieff MK. Available at: https://www.unicef-irc.org/ article/958-the-first-1000-days-of-life-the-brains-window-ofopportunity.html [Accessed on:16-08-2022]. 9. Journey of The First 1000 Days. Foundation for a Brighter Future. Rashtriya Bal Swasthya Karyakram. Ministry of Health & Family Welfare. Government of India. April 2018. Available at: https://nhm.gov.in/ images/pdf/programmes/RBSK/Resource_Documents/Journey_of_The_ First_1000_Days.pdf [Accessed on: 16-08-2022]. 10. Chapter 3: Addressing the Challenge of Hidden Hunger. Global Hunger Index. The Challenge of Hidden Hunger. Available at: https://www.ifpri.org/ sites/default/files/ghi/2014/feature_1818.html [Accessed on: 17-08-2022]. 11. FOGSI Focus. Nutrition In Women: Across Ages. Available at: https:// fogsi.org/wp-content/uploads/fogsi-focus/fogsi-focus-nutrition-inwomen-across-ages.pdf [Accessed on: 17-08-2022]. 12. Gernand AD, Schulze KJ, Stewart CP, et al. Micronutrient deficiencies in pregnancy worldwide: health effects and prevention. Nat Rev Endocrinol. 2016;12(5):274–289. 13. Biesalski K. “Hidden hunger” – being full isn’t enough. Available at: https://www.nutri-facts.org/en_US/news/articles/_hidden-hunger_– being-full-isnt-enough.html [Accessed on: 17-8-2022]. 14.Ruel-Bergeron JC, Stevens GA, Sugimoto JD, et al. Global Update and Trends of Hidden Hunger, 1995-2011: The Hidden Hunger Index. PLoS ONE 10(12):e0143497.15. Harding KL, Aguayo VM, Webb P. Hidden hunger in South Asia: a review of recent trends and persistent challenges. Public Health Nutr. 2018;21(4): 785–795. 16. Muthayya S, Rah JH, Sugimoto JD, et al. The Global Hidden Hunger Indices and Maps: An Advocacy Tool for Action. PLoS One. 2013;8(6):e67860. 17. Nguyen PH, Kachwaha S, Tran LM, et al. Maternal Diets in India: Gaps, Barriers, and Opportunities. Nutrients. 2021;13(10):3534. 18. Beluska-Turkan K, Korczak R, Hartell B, et al. Nutritional Gaps and Supplementation in the First 1000 Days. Nutrients. 2019;11(12):2891. 19. Elmadfa I, Meyer AL. Vitamins for the first 1000 days: preparing for life. Int J Vitam Nutr Res. 2012;82(5):342-7. 20. Gomes F, Agustina R, Black RE, et al. Multiple micronutrient supplements versus iron-folic acid supplements and maternal anemia outcomes: an iron dose analysis. Ann N Y Acad Sci. 2022;1512(1):114-125. 21. Engle‐Stone R, Kumordzie SM, Meinzen‐Dick L, et al. Replacing iron‐folic acid with multiple micronutrient supplements among pregnant women in Bangladesh and Burkina Faso: costs, impacts, and cost‐effectiveness. Ann N Y Acad Sci. 2019;1444(1):35–51.